Abstract
Spleen dysfunction and susceptibility to pneumococcal infection is a well known feature in homozygous sickle cell disease (HbSS), whilst to date splenic function in hemoglobin SC disease (HbSC) has been poorly investigated. The aim of this study was to analyze spleen function in children with HbSC disease using a high-throughput validated method (1) and to examine if the current recommendations regarding pneumococcal risk are appropriate in this population.
Spleen function was evaluated using a flow cytometry quantification of red blood cells (RBCs) with Howell-Jolly bodies (HJBs), in a cross-sectional study of patients at steady state during an outpatient visit in an expert center. Quantification of HJB-RBCs was performed in children with HbSC disease aged < 10 years and compared to children with HbSS disease or healthy children of the same age groups, or splenectomized children. Additional exploratory analysis was performed according to age (under or above the age of 5 years old) and treatment group (hydroxyurea).
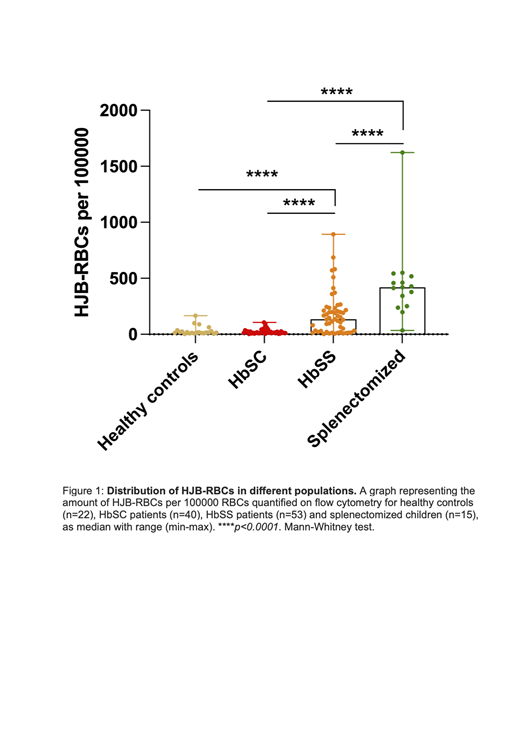
The median (Q1-Q3) HJB-RBCs count was 16 (11-28.25) /100.000 RBCs in 40 HbSC children (Figure 1). This result was not statistically different from the control group of 22 healthy children (p=0.96) nor in subgroups < or ≥ 5 years old, indicating that children with HbSC under 10 years have a preserved splenic function. Expectedly, the HJB-RBCs counts differed significantly from splenectomized children (419 (296-489)/100.000 RBCs, n=15, p<0.0001).
By contrast, among the 53 HbSS children, the median HJB-RBCs count was 134 (29-216) /100.000 RBCs, differing significantly from HbSC children (p<0.0001). In HbSS children, HJB-RBCs counts increased significantly with age (r=0.30, p=0.03), showing important variability among subjects but did not reach the level found in splenectomized patients suggesting that complete loss of spleen function occurs presumably later in a majority of children in this population. Treatment with hydroxyurea did not significantly impact HJB-RBCs counts in a subgroup analysis in HbSS children.
The result of this study suggests that spleen function in children under 10 years old with HbSC is not altered. The routine administration of prophylactic penicillin to young children with SC disease may therefore be questioned. Similarly, fever in children with HbSC under 3 years old may not require parenteral antibiotics as it is generally currently recommended by analogy to children with HbSS. Functional or anatomical asplenia in children with HbSC is delayed compared to those with HbSS at least after the first decade of life. Future large cohort studies using similar methodology will allow better evaluation of the pneumococcal risk in adolescents and adults with Hb SC disease.
Bibliography
(1) El Hoss S, Dussiot M, Renaud O, Brousse V, El Nemer W. A novel non-invasive method to measure splenic filtration function in humans. Haematologica. oct 2018;103(10):e436-9.
El Nemer: Hemanext: Consultancy.